When Is First Residual Limb Wrap Change After Surgery
LOWER-EXTREMITY AMPUTATIONS
AMPUTATION SITE VERSUS Role
Some of the older rules for limb length no longer apply in determining the level of amputation for prosthetic fit (12,thirteen,17). For instance, when a lower-limb prosthesis is fitted, adequate length of the residuum limb plus mod
components can often issue in significantly improve part than an
amputation that results in a longer lever arm with the utilize of more
basic and archaic components (16,xviii).
Partial Foot Amputation
The main advantage of a fractional human foot amputation is the
power to walk without a prosthesis. The disadvantages at this site
include the difficulty in making a cosmetic prosthesis with "toe off"
role, the uneven gait that results without toe-off function, the
tendency to develop an equinovarus deformity in the remainder foot
stump, and the limited foot components available (Fig. 122.1).
 |
| Figure 122.1. A: Midfoot amputation with a shoe insert prosthesis. B: An ankle–foot prosthesis for amputations through the hindfoot other than a Syme's amputation. (From Dee R, Mango E, Hurst LC. Principles of Orthopaedic Practice. New York: McGraw-Hill, 1989:365, with permission.) |
Syme'southward Amputation
Syme'south amputation retains the heel pad. The advantage of
this technique is that express ambulation is possible without a
prosthesis. Its disadvantages include a less cosmetic prosthesis due to
the thick talocrural joint required to adapt the stump, the express pes
components bachelor, and the express amount of energy storage within
these components (Fig. 122.2).
 |
| Figure 122.2. Syme's prosthesis with posterior cutout for donning the prosthesis. (Courtesy of the Joyce Center, Manhasset, NY.) |
Transtibial Amputation
In elective surgery where the amputation site tin can be
selected, it is preferable to accept enough space distally to incorporate
appropriate prosthetic components for all-time function and cosmesis, while
maintaining adequate length of the residual limb. Ideally, the length
of tibia from the mid-knee joint to the distal finish should exist no less
than 4 in. (10 cm) and no more than than 7 in. (17.75 cm). If the tibia is
too long, the pick of components is limited and cosmesis may exist
compromised. The space from the flooring to the end of the residual limb
(after the incision is closed) should be at to the lowest degree 12 in. (thirty.v cm), but
not if it volition get out the length of the tibia less than 4 in. (10 cm).
Through-the-knee Amputation
Through-the-genu amputation provides the potential of
end bearing in the prosthesis, a long lever arm, and condylar
intermission. A knee disarticulation is specially good for patients
with poor gait and neuromuscular control. Information technology is important in children
with growth potential who demand their distal femoral epiphysis to retain
stump length. The disadvantages of this technique include the limited
genu components bachelor (including a push button rotator), the differences
in the middle of rotation of the 2 knees, poor cosmesis due to the
large femoral condyles, and atrophy of the thigh that occurs with
condylar suspension. High-performance function is amend achieved with
a long transfemoral
amputation and a prosthesis with modern knee components.
Transfemoral Amputation
When in that location is a choice of amputation site, a infinite of four
in. (10 cm) from the human knee center to the distal cease of the residual limb
is optimum, equally long as this is not greater than one-third the length of
the femur. This space permits a greater pick of knee and other
components, and part and cosmesis are improved (Fig. 122.three).
 |
| Figure 122.3. |
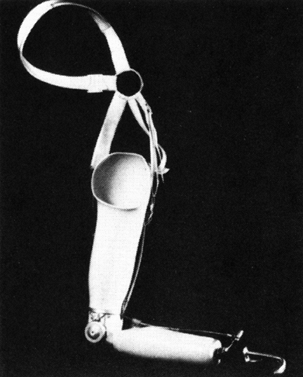
Hip Disarticulation and Hemipelvectomy Amputation
Lightweight components and flexible buckets/sockets have
improved comfort and reduced the workload of patients wearing these
types of prostheses (Fig. 122.4).
 |
| Effigy 122.iv. Endoskeletal prosthesis with cream cover for a hip disarticulation. (Courtesy of the Joyce Heart, Manhasset, NY.) |
PREPROSTHETIC CARE
The goals afterwards surgery for lower-extremity amputations in which there is a residual limb are listed in Tabular array 122.1.
These can be achieved through i of several methods: an immediate
postoperative prosthesis or serial wrapping of the residual limb with
an elastic bandage or an rubberband shrinker. The overall aim is to reduce
postsurgical edema. This in plough reduces postsurgical pain, minimizes
after phantom hurting, increases circulation (therefore hastening
healing), and prepares the operative site and residual limb for a
preparatory prosthesis. Where possible, acme of the afflicted limb
tin also assistance reduce edema, although this must be accompanied past
immediate aggressive physical therapy to prevent contractures of the
surrounding joints. When at that place is no remainder limb, the postsurgical
goals are fewer (Table 122.one). Methods to
reduce postoperative edema and prevent breakup of the incision in
patients include turning the patient onto the sound side and early
mobilization.
 |
| Table 122.1. Goals of Preprosthetic Care |
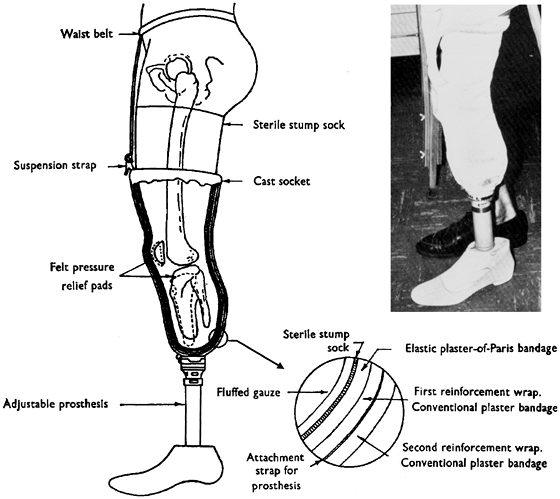
Firsthand POSTOPERATIVE PROSTHESIS
An firsthand postoperative prosthesis (IPOP) is a specialized dressing covered past a plaster bandage molded to provide
weight-bearing areas to enable patients to ambulate as before long as it is
applied. The IPOP incorporates an adapter into its distal cease that
has a removable pylon with a prosthetic foot attached.
An IPOP is intended to control edema, promote
ambulation, and forestall flexion contractures, as well as to keep
patients from "waking up without a leg." The prosthetist applies a
specially padded and molded cast in the operating room after the
surgical dressings have been applied. The advantage of this technique
is that the cast initially prevents postsurgical edema, promoting wound
healing and reducing hurting. The cast also protects the residual limb,
prevents flexion contractures in the surrounding joints, and molds the
residuum limb while compression is maintained. The difficulties with
this technique are that the cast loosens as shortly as the edema subsides
and the subsequent pistoning action can cause tissue breakup. The
bandage must either be continually replaced or exist removable so that
boosted socks or fillers tin be used to maintain compression. Other
difficulties involve the heaviness of the cast, which prevents motility
of the independent joints, impedes walking, and leads to muscle atrophy.
The cast must be removed to monitor wound healing, oftentimes needs to
exist reapplied to comprise compression, and is not corrective. Auxiliary
suspension may be required (Fig. 122.5).
 |
| Figure 122.five. |
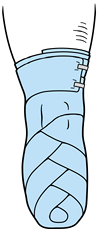
The advantage of an elastic compression cast is that
it tin be reapplied whenever it becomes loose and therefore compression
can exist kept abiding. Patients can be taught to wrap the limb, and
compression can be applied only in areas where it is needed (Fig. 122.6 and Fig. 122.7).
The problem with a pinch dressing is that information technology may be wrapped also
tightly, causing pain or tissue breakdown, or as well loosely to be
effective. Patients may have difficulty wrapping it themselves, and it
may cause window edema when applied incorrectly or unevenly.
 |
| Figure 122.vi. |
 |
| Figure 122.7. |
Elastic shrinkers, when applied correctly, provide
overall compression and allow wound monitoring. They may exist hard
to apply correctly in some individuals, however, and may not put direct
pressure over areas where it is needed (Fig. 122.eight).
 |
| Figure 122.viii. Rubberband shrinker for a transfemoral residual limb. (Courtesy of the Joyce Center, Manhasset, NY.) |
The choice of these diverse techniques depends on the
power and cooperation of a patient, the length of the limb, and
careful evaluation of the goals for the individual.
Secondary goals include the maintenance of range of
motion in the surrounding joints (hip and knee), prevention of musculus
atrophy, and emptying of pain. To achieve these, physical and
occupational therapy consisting of range-of-movement, stretching, and
strengthening exercises should exist initiated as soon as possible. An
early fit of the prosthesis will be beneficial.
RATIONALE FOR A PREPARATORY PROSTHESIS
A preparatory prosthesis is fitted to a patient while
the amputated limb undergoes normal maturational shape changes later on
surgery. Plumbing fixtures should be started after the sutures or staples accept
been removed and the incision has healed.
In the lower limb, the primary purposes of a preparatory
lower-extremity prosthesis include controlling postsurgical edema,
minimizing the loss of muscle mass and strength, preventing joint
contractures, and allowing patients to ambulate. Historically,
preparatory prostheses were made with the simplest components, worn
with prosthetic socks, and suspended with straps and belts. To
accommodate postsurgical shrinkage and musculus cloudburst of the residue
limb, the ply of the socks was increased until the size of the limb
stabilized, at which time the definitive prosthesis would exist
made. Withal, new socket materials and designs, along with
modern components and more ambitious training, promote the use of
remaining musculus so that subsequently postsurgical edema has subsided, there
is often little or no muscle atrophy. If advisable for an individual,
one of several types of suction break tin often be used as shortly as
the incision is completely healed, replacing the socks and belts. With
the employ of more sophisticated components, correct gait tin be taught
immediately to avert retraining once the definitive prosthesis has been
fit.
Later on the socket is carefully fitted and fabricated and
the components are aligned, patients should be taught how to use the
prosthesis. Limit ambulation to partial weight begetting, and check the
residual limb oft; graduate to total weight begetting as
tolerated. How long this takes will depend on the fit of the
prosthesis, as well equally the strength, coordination, ability, and
decision of the patient.
Although the remainder limb volition continue to mature and
change shape for the lifetime of individuals, the near dramatic changes
occur during the commencement three–6 months. Constantly monitor and change the
socket, or change the sock ply to suit these changes to maintain
fit. Make patients aware that this is quite normal. The definitive
prosthesis is made once these changes take stabilized.
PROSTHETIC FITTING AND ALIGNMENT
When fitting a first prosthesis, the prosthetic team
thoroughly examines a patient and evaluates the medical history. A
detailed explanation of the process of prosthetic fitting, preferably
accompanied past written materials, is given to the patient. A
prescription recommendation is sent to the referring physician by the
prosthetist with a asking for a letter of medical necessity. The
main concerns are comfort, part, and cosmesis. The prescription
recommendations depend on the patient's age, previous activeness level,
hoped-for outcome, length of residual limb, medical history, and
reimbursement limitations. The prescription should include blazon of
prosthesis (endoskeletal versus exoskeletal), type of intermission,
socket design, materials, pick of components, and corrective finish.
The condolement of the socket is always the primary business organization
and depends on the skill of the person taking the measurements or the
impression of the residual limb, as well as on the materials used.
Initially, measurements are taken, and a negative wrap of the residual
limb (or digitized equivalent; see beneath) is made. A positive model is
produced from the impression and modified, and a clear diagnostic
socket is formed over that mold. The diagnostic socket is fitted to the
remainder limb, the fit is checked, and any indicated changes are made
to the positive model, with refitting of the socket if necessary. A
flexible, total-contact socket is formed within a rigid frame, and the
chosen components are aligned so that the foot, knee joint, and and so on
are in a neutral alignment. The prosthesis is and then fitted and
dynamically aligned, and initial gait training is performed while the
alignment is fine-tuned. Subsequently the prosthesis is delivered to the
patient for trial utilize, a protective corrective encompass is fabricated, and
further alignment and fitting changes are made, equally necessary, on the
footing of continued functional test.
Although the majority of prosthetists take a cast of the
residuum limb and manually modify the positive mold to fabricate a
socket, an alternative method is the computer-aided
blueprint/computer-aided manufacturing (CAD/CAM) system. With this system,
information on the balance limb is converted into numerical data, read
into the figurer past a digitizer (commonly from a negative mold), and
converted into a three-dimensional prototype past commercially available
software. Modifications to this epitome are made by the prosthetist; the
information is then relayed to the attached carver, which produces the
positive model. Thereafter, the processes are similar regardless of
whether the manual or the CAD/CAM method is used: A difficult, articulate
diagnostic socket is formed over the model then fitted on the
residual limb. Weight-begetting surfaces and bony or sensitive areas are
checked, and whatsoever necessary modifications are made to the diagnostic
socket before the definitive 1 is fabricated.
Once the components have been assembled and
demote-aligned, a dynamic alignment must be done with the patient
wearing the prosthesis. There are two schools of thought concerning
alignment: Co-ordinate to i school, the prosthesis is aligned to
arrange whatever abnormalities in posture, such as flexion contracture,
whereas with
the
2d gradual corrections in alignment are made simultaneously with
aggressive rehabilitation of the patient, until a more correct
alignment can be obtained.
Frequent follow-upwardly visits are necessary later on delivery
of the prosthesis to make the corrections and adjustments that will
inevitably be needed equally a patient progresses. Information technology is important that
patients empathize that this is a normal process and that a plateau
volition eventually be reached where it will only be necessary to have
routine bank check-ups, unless a new prosthesis needs to be fabricated. They
must be informed of the importance of maintaining a stable body weight
and a regular do plan. Excessive gain or loss of weight
compromises fit and part of a prosthesis. Many of today's
components are designed for a weight range or activity level.
Endoskeletal versus Exoskeletal Prostheses
A endoskeletal prosthesis is made with an internal skeleton of components and a foam outer cosmesis (Fig. 122.9).
It is modular in design, thus permitting greater interchangeability.
The advantages of the endoskeletal are that changes in alignment can exist
made with ease at any fourth dimension during the life of the prosthesis to
suit changes in posture, gait, or growth. In the modular design,
individual components can exist changed without remaking the prosthesis.
The problems with this technique are that it is more expensive and may
require more than maintenance.
 |
| Figure 122.9. |
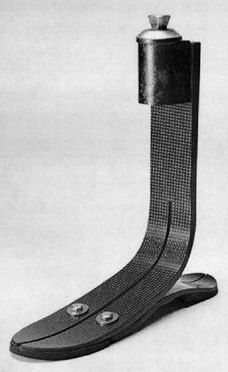
The exoskeletal prosthesis is often made of wood or polyurethane with a laminated rigid outer shell (Fig. 122.x).
Once fabricated, it has express adjustability without being
refabricated. It is less expensive and has a more durable cover than
the endoskeletal blazon. Its disadvantages include no postdelivery
accommodation–alignment changes, limited dynamic response capability,
and limited component choices. In addition, it is frequently heavier
than the endoskeletal prosthesis.
 |
| Figure 122.10. |
Suspension can be achieved with suction or a sleeve,
belt, or gage strap. The suction technique aims to reduce pistoning in
the socket, thus requiring less free energy expenditure during ambulation (Fig. 122.eleven).
It promotes venous return and gives patients the feeling that the
prosthesis is lighter. In addition, it eliminates the need for
uncomfortable belts and straps.
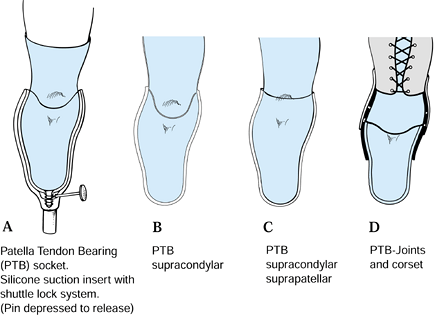 |
| Figure 122.11. Types of suspension for transtibial amputees. A: |
In the transfemoral amputation suction awarding, the
residual limb is drawn into the socket with an elastic cast or a
type of pull sock until the air is displaced through the distal valve
pigsty; a i-way valve is placed in the valve hole to prevent air from
reentering the socket (Fig. 122.3).
Although it seems easier to lubricate the residual limb and push button it
into the socket, the event is hammocking (stretching) of tissues on
the distal end and failure to get all the proximal tissue into the
socket.
In transfemoral or transtibial amputations, i of
several silicone or gel liners with a distal locking mechanism tin be
used. These are rolled upwards onto the rest limb, with the liner
property onto information technology; and the distal locking machinery attaches mechanically
to the prosthesis, creating an culling suction fit.
The sleeve technique is used for transtibial
awarding. The distal end of the sleeve fits over the proximal
portion of the prosthesis. The proximal end of the sleeve is and so
pulled up over the knee onto the patient's thigh. Information technology can human action as a
suction device if it is made of nonporous textile.
The belt suspension is used in transfemoral and
transtibial applications when suction suspension is not an choice. Information technology
can be used in conjunction with a socket interface, socks, or silicone
gel liner that has no locking mechanism.
The supracondylar cuff strap in used for transtibial
applications when suction is non an pick. It is sometimes used in
conjunction with a waist belt.
Socket Blueprint
The shape and fit of the socket is the single near
important factor in a successful outcome. Today's sockets are designed
to fit more anatomically and to provide total contact with the residual
limb. Increased suction on the distal end of the residual limb, due to
lack of contact, results in verrucous hyperplasia, if left uncorrected.
Under extreme circumstances, this can lead to localized infection or
cellulitis.
The sockets are usually made of flexible plastic and
surrounded by a rigid frame to support the weight-bearing areas. The
quadrilateral socket for the transfemoral amputee is being replaced by
i of several versions of ischium-containing designs. Containment of
the ischium within this type of socket provides pelvic stability and
promotes more normal femoral alignment and meliorate function of the
remaining intact musculature. Proprioception is also increased.
It is now possible to make more comfortable sockets for
college transfemoral, hip-disarticulation, or hemipelvectomy
amputations. The saucepan socket is made of laminated silicone or
flexible plastic supported by a rigid frame (Fig. 122.iv). The new families of silicone or gel socket liners have improved the comfort of sockets.
Pick of Components
Components that improve the comfort and function of the
prosthesis should exist used. It is our opinion that the more debilitated
a patient is, the greater is the need for aid from the prosthesis. The
question posed should be, "What tin can we provide to make walking easier
and more efficient for a person?" rather than making the assumption
that this person is not "a candidate for ambulation." The components
requiring consideration are the hips, the knees, and the feet.
The hip joints are express to single-axis joints with an extension assist.
Several types of knee joints are bachelor. The single-axis,
abiding-friction knee is the simplest design. The chief drawback for
this component is that ambulation is normal only at i speed for a gear up
amount of friction. The condom knee with constant friction is designed
so that the patient's weight locks the knee in the standing position.
The polycentric knee joint has hinges external to the prosthesis and
was originally designed for through-the-knee prostheses. It provides
better control during standing and the opinion stage of gait. The swing
phase may exist controlled mechanically or with a hydraulic cylinder.
Hydraulic knee joints, which are the nigh sophisticated on the marketplace
to date, control both swing and stance stage and are
velocity-sensitive. Tabular array 122.2 specifies the indications for employ of the diverse types of prostheses, together with advantages and disadvantages.
 |
| Table 122.2. Genu Joints for Above-Knee joint Prosthesis |
The prosthetic ankle–foot systems comprise several chief
groups: articulated ankle joints, dynamic-response and energy-storing
foot, and nondynamic-response and/or free energy-storing anxiety. The simplest
and cheapest combination is the nonarticulated ankle and the
nondynamic-response foot, called the solid ankle-cushion heel (SACH)
foot; it is also the least efficient.
The combination of a solid ankle and a dynamic-response
pes allows maximum loading of the toe department of the foot during
"rollover." Similar to the action of a coiled spring, when the pressure
or loading is removed, the toe section springs back to provide
push button-off. The most extreme version of this is institute in a human foot–ankle and
shank fabricated of carbon fibers, in which the loading action or energy
storage is likewise carried out in the shank. The method of loading the toe
must be taught, or the benefits volition not be experienced. In fact, users
may complain that the toe is too stiff, and pass up the foot.
An articulated talocrural joint articulation, useful for people who spend
considerable time walking on uneven ground, is heavier than other
prosthetic anxiety and requires more maintenance. An added disadvantage is
that even if it is combined with a dynamic-response human foot, the action of
the ankle precludes loading the toe to provide push-off. The diverse
options for lower-extremity prosthetic components are shown in Figure 122.12.
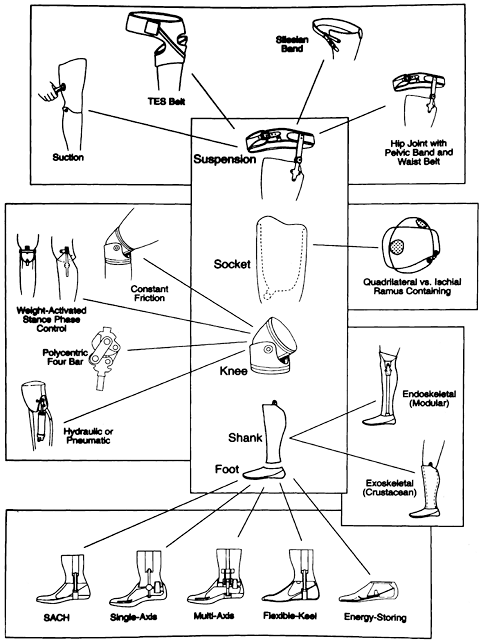 |
| Figure 122.12. Choice of components for the transfemoral amputee. (From Braddon RL. Physical Medicine and Rehabilitation. Philadelphia: W.B. Saunders, 1996:307, with permission, University of Texas Wellness Science Center at San Antonio.) |
REHABILITATION AND Preparation
A successful outcome depends as much on rehabilitation
and preparation as it does on the fabrication and fitting of a prosthesis.
Studies show that energy expenditure during ambulation is higher for
amputees than for nonamputees (2,6,7,9,10,14,15,xix).
Factors affecting energy expenditure include the length of the residual
limb, unilateral or bilateral amputation, the reason for amputation,
the choice of prosthetic components, the weight of the prosthesis and
whether the weight is concentrated distally or proximally, the
efficiency of the suspension aids for the prosthesis, the symmetry of
the gait, the country of the cardiovascular system, the patient's historic period,
and the general country of concrete fitness (5,11).
The net energy cost of ambulation, or the corporeality of oxygen required per kilogram of body weight per meter walked (ml O2/kg/k),
is higher than normal in nigh untrained amputees and increases equally the
amputation level gets higher. In addition, the preferred speed of
walking becomes slower (8). The weight of the
prosthesis can contribute to this increased free energy cost, particularly
if the extra weight is distal. Suction intermission can brand a prosthesis
feel lighter, while pistoning betwixt residual limb and socket creates
a pendulum effect. Conscientious choice of components is therefore very
of import. A less symmetric gait also requires more energy. Elderly
individuals who accept an amputation for vascular reasons are less
efficient partly because of the crumbling process merely also equally a outcome of
arteriosclerotic center disease, peripheral vascular disease, or
diabetes, which all inhibit the efficient transfer of oxygen to the
muscles.
Start balancing, stretching, and muscle-strengthening
exercises as presently as possible after amputation to maintain flexibility,
foreclose flexion contractures, and preserve muscle strength and mass. In
improver, brand an aerobic conditioning program a part of the
rehabilitation process whenever possible. This combination will accept
the dual effect
of
strengthening the cardiovascular system then that there is more than efficient
transfer of oxygen and building up muscles to utilize that oxygen (8). In one case a prosthesis has been fitted, patients should practice all physical therapy and practice programs with the prosthesis on.
Correct-gait training starts with the first step taken
in the prosthesis. Even if just fractional weight bearing is allowed,
encourage amputees to stand directly and accept even strides. It is
easier to teach someone correctly from the get-go than to try to
correct a bad habit later, only as information technology is easier to prevent a flexion
contracture than to correct information technology. Although walking frames are frequently
used, particularly by the elderly, they accept the disadvantage of
encouraging users to walk unevenly. Typically, a long footstep is taken
with the audio side to the front of the frame, and the prosthetic side
is then simply brought even with the sound side. If a walker must be used
for stability, information technology should exist moved frontward before each footstep to permit
room for the feet to exist placed sequentially 1 in front of the other.
Fear of losing residual and falling is the main business organization
of new amputees. Functional muscle-strengthening exercises—those that
are carried out standing on the prosthetic side while exercising the
sound side—are as important as exercises carried out on the affected
side.
We have observed that, unless taught otherwise, many
amputees volition stand up and walk with their afflicted-side hip behind their
sound-side hip, even though the shoulders will remain directly. The
result is that the stride length is uneven, with the step taken with
the prosthesis beingness longer than that with the sound side. Apply of an
energy-storing/dynamic-response pes volition in effect prevent loading of
the toe and the resulting toe push button-off. It has therefore been our
practice to gait-railroad train our clients in the following way:
-
At heel strike on the affected side,
contract the muscles on that side from the gluteals to the stop of the
residual limb and push downwards and back. -
Move the affected hip forwards until the
pes is flat on the floor while rolling forward (not upward) onto the toe
of the sound side and starting the sound-side swing phase. -
Move the affected hip further forward,
feeling the stretch in the hip flexors, compressing and loading the
prosthetic toe while completing the swing phase of the audio side. -
At heel strike on the sound side, relax
the muscles on the affected side. The prosthetic toe will button off,
initiating a knee bend and afflicted-side swing-through.
In this way, the patient'south ain body weight is doing the
work of loading the prosthetic toe. It is also important to maintain
normal upper-body motility, that is, equal arm swing and torso
rotation. Although it seems to exist very hard piece of work initially, the
result is a more even gait pattern and less piece of work. Effigy 122.13 and Figure 122.fourteen depict the appropriate activeness of the muscles during gait for transtibial or transfemoral amputation.
 |
| Figure 122.xiii. Muscle action in the flexors and extensors of the hip and knee during the gait cycle for a transtibial amputee. |
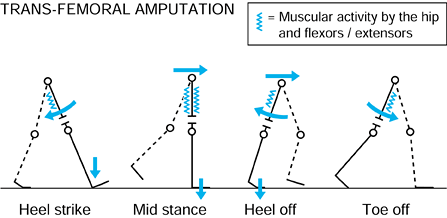 |
| Figure 122.xiv. Muscle activity flexors and extensors of the hip in a transfemoral amputee during the full-gait cycle. |
Unless contraindicated, a supervised aerobic
conditioning program will improve the endurance of all lower-extremity
amputees—information technology is non only for athletes. In our experience, as long as a
prosthesis fits well, a tailored practise program can exist undertaken past
individuals with diabetes and circulatory insufficiency, and they volition
benefit. Stationary bicycles, rowing machines, or upper-body ergometers
tin all be used, although the treadmill is the piece of equipment of
choice because it also improves walking. Ideally, in improver to
stretching and muscle-strengthening exercises, these individuals should
practise for a minimum of 20 minutes at least iii times per week at
an elevated heart rate determined by their physicians.
GAIT ANALYSIS
After a patient has had some early on experience in the
prosthesis, members of the prosthetic team must observe the patient's
gait on a direct-level walkway to be certain that gait abnormalities
are not due to inadequate rehabilitation or improper plumbing fixtures or
alignment of the prosthesis. Table 122.3 and Tabular array 122.4
provide an outline of commonly observed gait abnormalities, a
description of their characteristics, and common causes that require
correction.
 |
| Tabular array 122.3. Gait Analysis of the Transtibial Amputee |
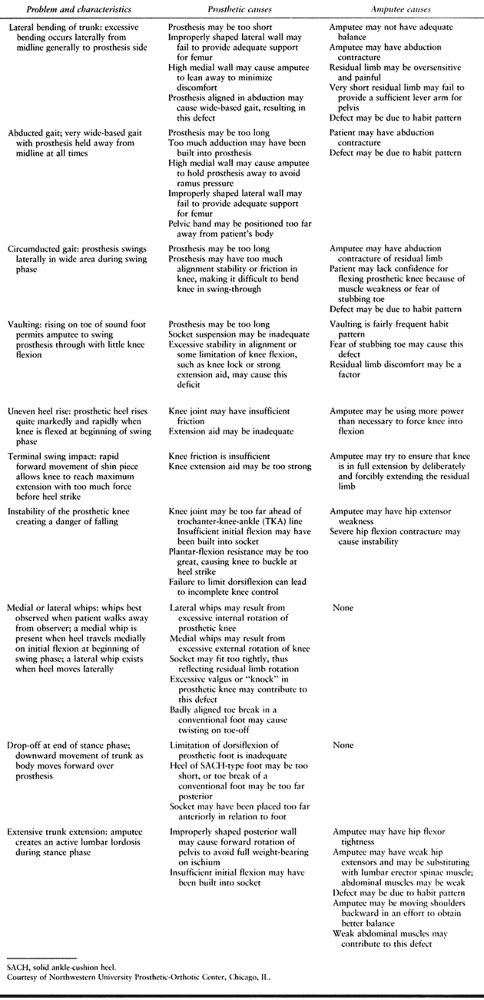 |
| Table 122.4. Gait Assay of the Transfemoral Amputee |
UPPER-EXTREMITY AMPUTATIONS
AMPUTATION SITE VERSUS Function
Upper-extremity amputations include wrist
disarticulation, beneath-elbow amputation, elbow disarticulation,
above-elbow amputation, shoulder disarticulation, and forequarter
amputation. Wrist disarticulation has the greatest range of extremity
movement: flexion, extension, pronation, and supination. It also has a
long lever arm for strength and support of distal components, and
increased proprioception and office. However, it is more hard to
fit with a myoelectric hand and wrist, and the resulting fit is ofttimes
longer than the sound side. The choice of components is limited.
The beneath-elbow amputation provides anatomic ability to
pronate and supinate, has a wider range of components available, and
tin achieve equal length with the sound side. The pick of a
myoelectric or body-powered prosthesis is available. This amputation
has less range of move, a shorter lever arm, and less proprioception
and part than the wrist disarticulation. Anatomic pronation and
supination decrease every bit the length of the remainder limb decreases.
The elbow disarticulation has a long lever arm and
potential increased prosthetic range of motion, for the
shoulder-to-elbow portion, when fitted with a prosthesis, will
be
longer than the opposite extremity than with the above-elbow
amputation. The increased length at the elbow is due to the components,
but casual observers do not find the discrepancy. Choice of elbow
components is limited to trunk-powered devices.
The above-elbow amputation has a better selection of elbow
components, either myoelectric or body-powered. It has a short lever
arm to back up distal components and a express potential range of
motion.
Shoulder disarticulation and forequarter amputation
leave patients with significant disability. The shoulder
disarticulation has a very express range of motion, and the prosthesis
is cumbersome and heavy. It is oft used primarily for cosmesis.
The forequarter amputation also has a limited range of motion. The
prosthesis is even more cumbersome and heavy, and pause is
peculiarly difficult. The more than distal the amputation in the upper
extremity is, the more functional the outcome and the better the
cosmesis will exist.
PREPROSTHETIC Care
The goals of preprosthetic care for upper-extremity amputations are the same as those for lower-extremity amputations (Table 122.1).
Immediate POSTOPERATIVE PROSTHESES
An IPOP applied to the upper-extremity controls
postsurgical pain and edema, improving circulation through reduced
edema. Patients do good psychologically past "waking upwards with a hand and
arm."
In amputations with a residual limb, a preparatory
upper-extremity prosthesis can protect the residual limb from injury,
preclude and treat contractures in the contained joints, and initially
mold the residual limb. Patients maintain some two-handed part and
receive training in the use of a prosthesis. Information technology also allows assessment
of a patient's motivation. Information technology can be removed for wound care and helps
maintain body symmetry. The IPOP is usually worn just for 2–half-dozen weeks
later on surgery. It is body-powered rather than myoelectric, and because
of its weight, it uses a terminal claw device rather than a mitt.
Withal, the plaster cast of the IPOP is heavy and
prevents movements of contained joints, resulting in muscle cloudburst. If
the bandage becomes loose, it tin cause tissue breakup, particularly if
information technology is resting on the transradial area or other proximal joint. The cast
is also prone to fall off, particularly with transhumeral amputations,
unless auxiliary break is used. Use of a cast likewise prevents
monitoring of the incision. Another problem with this technique is that
the terminal claw device is non cosmetic. An IPOP cannot exist applied
over extensive skin grafting and is not useful on very short residual
limbs.
The rationale for upper-extremity preparatory prostheses is the same as that for lower-extremity preparatory prostheses.
PROSTHETIC FITTING
Rejection of upper-extremity prostheses is more common
than for lower-extremity prostheses, with rejection rates increasing
the more proximal the amputation site is. If prosthetic fitting is not
done early, the client tin can become and then adept at doing tasks with one hand
that a prosthesis may seem cumbersome and heavy.
Length, status, force, and range of motion of the
residue limb are the determining factors in the choice of a prosthetic
organisation. Personal preference and motivation also play a role.
Preservation of length of the residual limb in
upper-extremity amputations is critical for maximum function. This
differs from the principles for the lower-extremity, where components
tin can be more than functional and a long residuum limb length is not ever
beneficial.
Upper-extremity prostheses involve several choices:
-
Passive, in which the position of the concluding device or more proximal components is inverse with a contralateral mitt
-
Torso-powered, in which gross torso movements activate cables for function
-
Myoelectric, which is bombardment-powered and computer-driven
-
Hybrid arrangement, which is a combination of torso-powered and myoelectric
Table 122.v delineates the advantages and disadvantages of these diverse options.
 |
| Table 122.5. Advantages and Disadvantages of Diverse Upper-limb Prostheses |
Passive Prosthesis
A passive prosthesis can exist used for individuals who
want nigh life-like cosmesis or who take a high-level amputation and
want a lightweight arm for cosmetic reasons. Passive prostheses are
lightweight and nonfunctional. Cost depends largely on corrective terminate.
Off-the-shelf cosmetic covers are relatively inexpensive, while nearly
life-similar silicone covers are expensive.
Torso-powered Prosthesis
In a body-powered prosthesis, the components are
controlled by gross body movements through a system of straps and a
harness that also doubles as a suspension help. Stainless steel cables
are attached to the straps proximally and to parts of the terminal
device distally. If the amputation is proximal to the elbow articulation, the
cablevision will go through an elbow flexion attachment first. Torso
movements, such as a shoulder shrug or scapular abduction, put tension
on a cable, causing a response. A series of movements initiates
flexion, extension, and locking of the elbow, after which the final
device can be activated (Table 122.6). If distal, the cables just control the terminal
device. The body-powered prosthesis does non depend on a battery for
power, has a quicker component reaction time, and is less expensive
than the myoelectric. In that location is feedback from the cable, and it is more than
durable and easier to maintain. Conversely, a body-powered prosthesis
is at risk for repetitive injury of the activating muscles and joints,
has express pinch-force command for an involuntary final device, and
tin cause irritation to the skin of the contralateral side from the
harness.
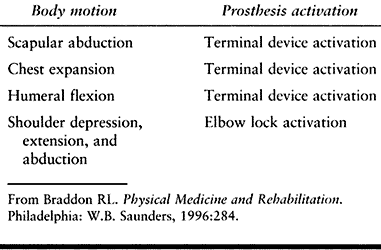 |
| Table 122.6. Body Command Motions Typically Used for Prosthesis Activation |
Myoelectric Prosthesis
Myolectric prosthetic components are controlled by
voluntary muscle action via an electronic bespeak. The signal is picked
up and amplified by electrodes placed over the musculus fibers and so
downloaded to a computer to provide a specific function.
To decide whether a patient is a candidate for this
type of prosthesis, myoelectric testing is washed, before the components
are chosen, to decide the maximum threshold available from the
muscles. A myoelectric prosthesis provides good cosmesis and does non
require a harness to exist activated. It has increased range of motion and
avoids repetitive-motility injury; it also has increased anatomic
function and voluntary wrist rotation. To its disadvantage, a
myoelectric device has a slower response fourth dimension and increased weight
distally, as well equally higher maintenance. Information technology is battery-dependent and
less durable and has a longer down time for repairs. In addition,
myoelectric devices are expensive, require longer training, and are
less adaptive and not waterproof (Fig. 122.15).
 |
| Figure 122.xv. |
Hybrid Organisation
The hybrid system has a combination of trunk-powered and
myoelectric components, such as a body-powered elbow and a myoelectric
paw. This combination reduces the weight of the prosthesis and the
expense.
Choice of Components
Types of Break
The socket design depends on the type of intermission used—suction, bony lock, or harness—and the socket fit.
Total-suction intermission is used for wrist
disarticulation and above- or below-elbow amputations. Information technology is more
secure, provides greater proprioception, reduces harnessing, and
enables pronation and supination where anatomically possible. With
full-suction intermission, the prosthesis feels lighter. However, it is
more hard to put on, especially for bilateral amputees, and
difficult to fit for short above- or beneath-elbow limbs. In improver, information technology
may be more expensive than other choices. A suction liner can be used
for in a higher place- and beneath-elbow prostheses. It is easier to put on than total
suction only may crusade skin irritation. Still, it is not as secure equally
full suction and is more than expensive.
Bony-lock intermission tin be used with or without socks
for wrist disarticulation and below-elbow prostheses. It is easy to put
on and remove. Its disadvantages are that it can cause muscle atrophy
and prevents pronation and supination in below-elbow amputees (eight).
Harness break tin be used for all upper-extremity
prostheses. It is less expensive and more reliable than other
suspensions, and the merely choice for a shoulder disarticulation or
forequarter amputation. The problem is that it is irritating to wearable
and is less cosmetic.
Terminal Devices
Apart from advent, weight is a main factor to exist
considered in the choice of a terminal device. Hooks are lighter, have
less of a pendulum effect, and are less tiring to apply. One choice is to
employ a claw for daily activities and to attach a hand whenever cosmesis
is more than of import. The passive device is nonfunctional and for cosmesis
simply. Both the body-powered hook and trunk-powered hand are voluntary-
or involuntary-closing devices. The myoelectric hand is battery-powered
and computer-driven. It has specific adaptive equipment, such as for
sports, tools, and and so forth.
The master groups of wrist units are body-powered and
myoelectric. Myoelectric devices can pronate and supinate and are
motor-driven. In elbow units, the main groups include passive,
trunk-powered, and myoelectric devices. In shoulder units, there is only
a manual unit.
Typical transhumeral and transradial body-powered prostheses are depicted in Effigy 122.xvi and Figure 122.17.
 |
| Effigy 122.sixteen. Typical torso-powered prosthesis for a transhumeral amputee (harness non shown). (From D'Astous J, ed. Orthotics and Prosthetics Assimilate, Canada: Edahl Productions Ltd, 1981:153, with permission.) |
 |
| Effigy 122.17. Typical body-powered prosthesis for a transradial level amputee. |
REHABILITATION AND Grooming
Institute occupational therapy every bit soon as possible to
maintain body symmetry, prevent flexion contractures, reduce surgical
edema, and prepare the residuum limb for the prosthesis. Early fitting
of a prosthesis and promotion of 2-handed function reduce the
rejection charge per unit. Strengthening exercises assist counteract the pendulum
effect of the concluding device. In addition, if myoelectric components
are used, patients may demand exercises to improve their power to
contract and cocontract the muscles chosen for the electrode site.
Reckoner programs are used to help in preparation patients. Activities of
daily living must be taught before a patient becomes expert at doing
these tasks unmarried-handedly; otherwise the prosthesis may feel
cumbersome.
For both upper- and lower-limb amputees, the resources
necessary for success are not always available. Reimbursement issues
keep to present considerable problems for both prosthesis and
rehabilitation costs. In addition, a patient sometime enough to receive
Medicare cannot learn to walk in the limited concrete therapy sessions
immune for gait preparation at either outpatient or private physical
therapy facilities. The reimbursement allowed by some insurance
companies for one prosthesis per lifetime is not sufficient when the
patient is a child built-in with a limb deficiency. Often, less functional
components are used, purely on the footing of toll. In addition,
prosthetists take different levels of skills.
![]() PITFALLS AND COMPLICATIONS
PITFALLS AND COMPLICATIONS
SKIN PROBLEMS
Proper prosthetic fitting and a good training program to
gradually suit amputees to their prosthesis and teach them how
to intendance for it and their skin will avoid most skin bug. The
rest limb and socket must be done daily. Areas of separate-thickness
peel graft practice not tolerate pressure, specially if over bony
prominences. They may eventually require revision if modification of
the socket is not successful in preventing problems. Painful bursas tin can
usually exist managed by modifications of the socket, but occasionally
problematic bony prominences will crave removal.
Fungal peel infections are all-time avoided by cleanliness,
keeping the socket and skin as dry out as possible, and, when necessary,
application of typical fungicides. Folliculitis usually results from
sweating, poor hygiene, and pistoning in the socket caused past a poor
fit. These problems usually reply to good skin care. If folliculitis
progresses to abscess, it may require incision and drainage, with
limited prosthesis employ until healing occurs.
CHOKE SYNDROME
Proximal restriction in the socket with lack of total
contact can lead to edema in the stump, which can lead to hemosiderin
deposition and the eventual development of verrucous hyperplasia. This
problem is preventable through good prosthetic fitting that achieves
full contact in the socket.
Pain
Hurting over surgical scars or bony prominences or from
neuromas should initially be addressed with socket modifications. If
modifications are unsuccessful, then surgical intervention may exist
required (encounter Chapter 120 and Chapter 121).
Most all adult amputees have an epitome and awareness of the amputated
function known every bit "phantom sensation," which usually declines with time. On
occasion, this will exist accompanied by hurting in the phantom. Rule out any
prosthetic or surgical causes of pain, as these may aggravate phantom
hurting. Referral to a pain management middle for medicinal therapy,
transcutaneous electrical stimulation, lumbar sympathic blocks, and
other such interventions may be useful. Potent psychosocial support for
patients is important.
CONTRACTURES
It is important to emphasize to patients the critical
part of early rehabilitation and exercises to build strength and
prevent flexion contractures. Minor contractures of upward to 10° tin can
usually exist accommodated in the prosthesis and crave no special
treatment. Hip and knee flexion contractures greater than 25° interfere
with prosthesis fitting and volition result in an unfavorable posture and
gait design. Surgical release is sometimes necessary if these do not
respond to nonoperative treatment.
PSYCHOSOCIAL MALADJUSTMENT
Amputee support groups and peer counseling are very
helpful for patients sustaining amputations in accepting their new body
image and adjusting to their new state of affairs. Open up give-and-take of their
bug and concerns in a group or mentor setting is helpful.
Resource
The Amputee Coalition of America and National Limb Loss
Information Middle (toll-free: 1-888-AMP-KNOW) is a national
organization that is helpful for new amputees. This center has an
data hotline and tin can help find a local support group and peer
visitor, as well as providing appropriate pamphlets, magazines, and
videos and a list of certified prosthetists in their area.
To be certified by The American Board for Certification
in Prosthetics and Orthotics, Inc., today'southward prosthetists must meet
sure educational and professional standards. These include a
available's caste and supervised internship, likewise as passing a
national certification examination followed past mandatory continuing
didactics. Every bit a result of constantly changing engineering science, amend
outcomes can be realized when prosthetists have input into the
prescription request based on the initial prosthetic evaluation.
Source: https://teachmeorthopedics.info/principles-of-amputee-prosthetics/
Posted by: dennisalannow.blogspot.com


0 Response to "When Is First Residual Limb Wrap Change After Surgery"
Post a Comment